
I'm genuinely excited right now.
Not "content creator excited." Not "this will make a good newsletter" excited. Actually, emotionally fired up in a way that's hard to put into words.
Because I just watched something happen with my mom that I wasn't sure was possible.
She's had Hashimoto's and hypothyroidism for over twenty years. Two decades of Levothyroxine adjustments, chronic fatigue, joint pain, and doctors telling her this is just how it's going to be. Manage the symptoms. Accept the limitations. That's the deal.
Her HPT axis—the hypothalamic-pituitary-thyroid feedback loop that controls everything—had reached what researchers call a "steady state of exogenous reliance." Translation: her body had given up on making its own hormones and just depended on the daily pill.
Until last week.
Her doctor looked at her bloodwork and said something she's never heard in twenty years: "We're lowering your dosage."
But here's what's got me emotional about this.
It's not just the labs. It's watching her come back to life. There's this spark in her eyes that I honestly forgot existed. She's got energy again. She's moving without pain. People are stopping her constantly asking what she's doing differently.
When I asked her what she thinks made the difference, she said:
"The only thing I've really changed is the peptide stack you put me on."
Same diet. Same lifestyle. Same stress levels. The only variable? Four months of MOTS-c and GHK-Cu.
I need to break down exactly why I think this worked—and I mean really break it down. Because there's a mechanism here that makes complete sense when you understand what these peptides actually do at a molecular level.
The Protocol
Two peptides. Consistent application. Patience.
Now let me take you inside the biology.
Why Levothyroxine Has a Ceiling
Here's the standard Hashimoto's playbook: Your immune system attacks your thyroid follicular cells. Your thyroid stops producing adequate T4. Your doctor prescribes Levothyroxine to replace what your body can't make.
Does it work? Yes—it keeps you functional.
But Levothyroxine does nothing to address the autoimmune attack. It doesn't repair mitochondrial dysfunction. It doesn't reduce chronic inflammation. It doesn't restore cellular sensitivity to the hormones you're taking.
For twenty years, my mom was essentially topping off a leaky tank instead of fixing the hole. The medication maintained her—but "maintained" isn't the same as "improved."
This is where MOTS-c and GHK-Cu change the equation. And there are four distinct mechanisms that could explain why her doctor is now lowering her dose for the first time ever.
Mechanism 1: Metabolic Substitution (MOTS-c)
MOTS-c is a 16-amino acid peptide encoded in the mitochondrial 12S rRNA gene. It's what researchers call a "mitokine"—a mitochondrial hormone that enters circulation and affects distant organs throughout the body.
Here's the key pathway: Folate → AICAR → AMPK.
MOTS-c inhibits the folate cycle, which causes AICAR to accumulate. AICAR then activates AMPK—the "metabolic master switch" that controls how your body uses energy.
When AMPK is activated:
GLUT4 transporters move to cell membranes, increasing glucose uptake
Fatty acid oxidation increases
Mitochondrial uncoupling proteins (UCP1 and UCP3) ramp up thermogenesis
Here's why this matters for thyroid patients:
In hypothyroidism, your basal metabolic rate tanks because thyroid hormones are required to stimulate the mitochondrial respiratory chain. T4 basically sets the "idle speed" of your cells.
MOTS-c may act as a metabolic adjuvant—doing the work that thyroid hormone was previously required to stimulate. If global energy expenditure and thermogenesis are restored through MOTS-c-driven mitochondrial activity, the physiological demand for exogenous T4 decreases.
Less demand = dose-sparing effect.
The body doesn't need as much synthetic hormone because the cellular machinery is now working more efficiently on its own.
Mechanism 2: Enhanced Peripheral Sensitivity (GHK-Cu)
Thyroid hormone action isn't just about circulating levels of T4 and T3. It's about receptor density, receptor sensitivity, and transporter efficiency.
Chronic inflammation and oxidative stress—hallmarks of aging and long-term autoimmune conditions—lead to what's called "thyroid hormone resistance." Your tissues fail to respond adequately to the hormones that are present.
GHK-Cu is a tripeptide that modulates approximately 4,000 human genes—roughly 31% of the genome.
Among its documented effects:
Suppresses NF-κB (master inflammatory pathway)
Reduces TNF-alpha and IL-6 (inflammatory cytokines)
Enhances Superoxide Dismutase activity (antioxidant defense)
By reducing the "inflammatory noise" in the cellular environment, GHK-Cu may improve the binding affinity of T3 to its nuclear receptors.
The result: The same circulating hormone produces a stronger biological effect. You need less T4 to achieve the same outcome because your tissues are actually responding to it now.
Mechanism 3: HPT Axis Recalibration (MOTS-c)
This one is critical—and it's backed by animal research.
Studies show that MOTS-c administration can decrease serum TSH, T3, and T4 levels. When MOTS-c was infused in rodent models, it increased peripheral energy expenditure via UCP1/UCP3 while simultaneously suppressing the central signal for thyroid hormone production.
What does this mean?
MOTS-c may be signaling to the brain: "Energy requirements are being handled through mitochondrial pathways—we don't need as much thyroid output."
The pituitary responds by reducing TSH. When a physician sees lower TSH on bloodwork, standard clinical guidelines say to lower the medication dose to prevent over-replacement.
In this scenario, the medication reduction is a direct response to a peptide-induced shift in the HPT axis set-point. The feedback loop has been recalibrated.
Mechanism 4: Glandular Regeneration (GHK-Cu + MOTS-c)
This is the most intriguing possibility—and the one that gets me excited.
The thyroid gland may actually be repairing itself.
GHK-Cu is known to stimulate stem cell proliferation and tissue remodeling in multiple organs. Since thyroid follicles are composed of epithelial cells that can regenerate, GHK-Cu may facilitate the repair of follicles that were previously dormant or damaged by two decades of autoimmune activity.
Here's the supporting evidence:
GHK-Cu increases "stemness" markers in basal cells (p63 expression). It activates the ubiquitin-proteasome system, helping cells clear damaged proteins that accumulate during chronic illness. It literally resets the "genomic environment" toward repair mode.
Meanwhile, MOTS-c has demonstrated the ability to regulate T-cell differentiation—promoting regulatory T-cells (Tregs) and inhibiting the autoreactive T-cells that drive autoimmune destruction.
For someone with Hashimoto's, this shift toward immune tolerance could halt the chronic attack on the thyroid, allowing remaining tissue to recover its hormone-producing capacity.
The Copper Connection (Often Overlooked)
GHK-Cu delivers bioavailable copper directly to tissues. This matters more than most people realize.
Copper is an essential trace element for thyroid function:
Required for enzymes involved in T4 → T3 conversion
Integral component of Superoxide Dismutase (protects thyroid from oxidative damage)
Positively correlated with thyroid hormone levels in research
Studies show a negative relationship between copper and TSH—as copper levels optimize, TSH tends to decrease because hormone synthesis and feedback improve.
GHK-Cu may be addressing a subclinical copper deficiency that standard medical evaluations don't catch. By optimizing the catalytic environment for thyroid hormone production, it supports a more efficient endocrine system that requires less external supplementation.
The Software/Hardware Model
Here's how I think about this combination:
MOTS-c = Software Update. It handles metabolic signaling, energy flux, and the communication between mitochondria and nucleus. It recalibrates the feedback loops.
GHK-Cu = Hardware Repair. It addresses glandular tissue integrity, genomic stability, and structural damage accumulated over twenty years.
When you update both simultaneously, the system can finally operate the way it was designed to.
My mom spent two decades with corrupted software running on damaged hardware. The Levothyroxine kept the system functional—but it couldn't fix the underlying problems.
These peptides addressed what the medication never could.
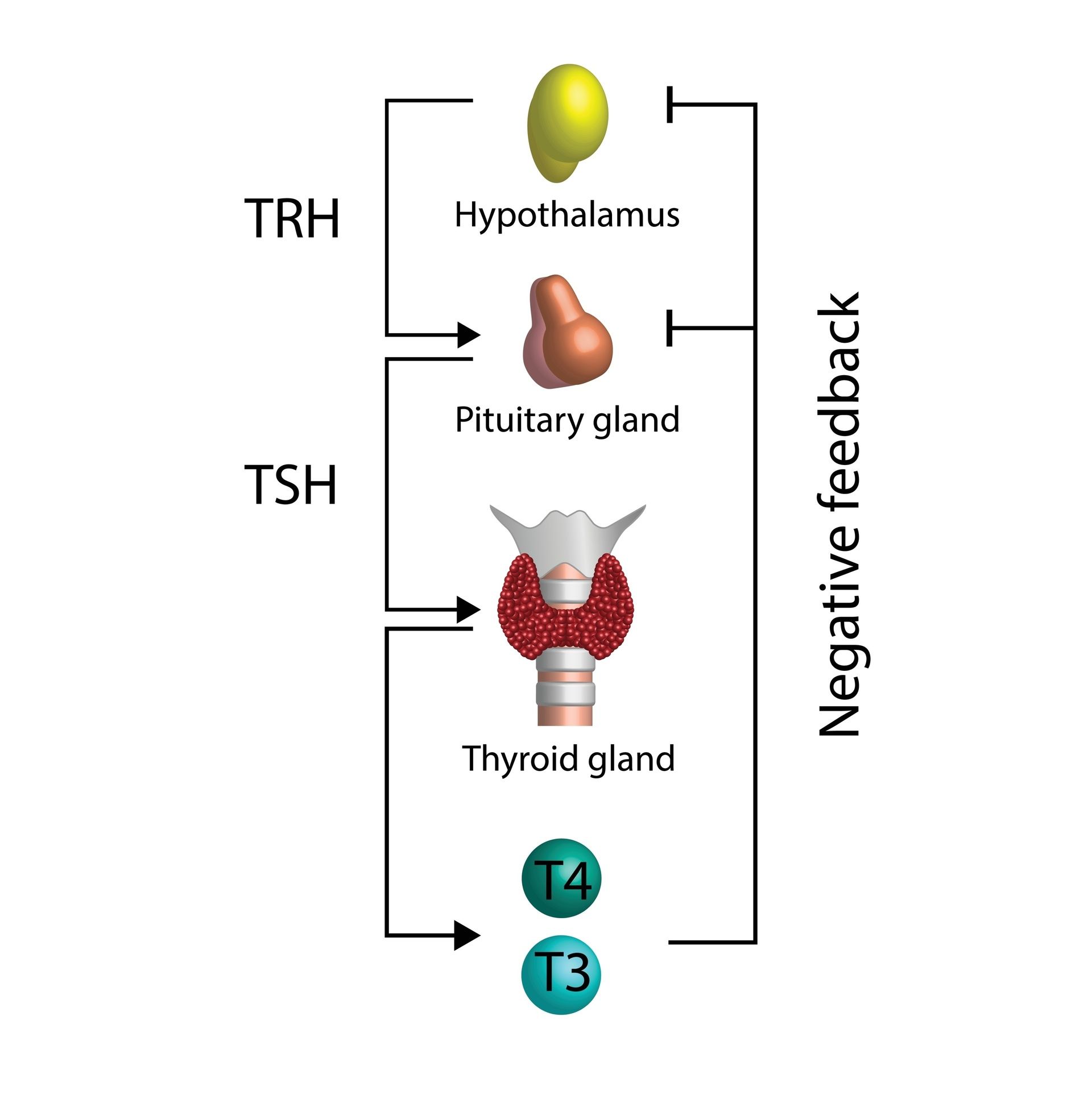
The HPT Axis: Your Body’s Internal Thermostat
What I'm NOT Saying
Let me be clear.
I'm not saying peptides cure Hashimoto's. I'm not saying throw out your Levothyroxine. I'm not saying this protocol will work identically for everyone.
My mom is still on medication. She's still working with her doctor. She's still getting regular labs. The peptides are working alongside conventional treatment—not replacing it.
What I am saying is this:
For the first time in twenty years, her trajectory changed. Not "managed." Not "maintained." Actually improved.
That's not a miracle. That's what can happen when you address root causes—mitochondrial dysfunction, immune dysregulation, chronic inflammation, tissue damage—instead of only replacing the missing hormone.
If This Resonates
If you or someone you love is stuck in that same twenty-year loop—autoimmune thyroid issues, chronic fatigue, doctors who only offer maintenance—this might be worth exploring.
Do your research. Get your labs. Work with practitioners who understand peptides. Make informed decisions.
But don't let anyone tell you that "managing symptoms forever" is the only path available.
If you want to run a similar protocol, I've attached the Limitless Life Nootropics links use code LEE20 for 20% off. I've also listed my other trusted peptide partners below if you want to compare sourcing options.
Talk soon,
Lee
Going to go hug my mom now.
Peptide Community & Member Perks
FURTHER READING & RESEARCH SOURCES
For those who want to dig deeper into the science behind this newsletter, here are the peer-reviewed studies and resources I referenced:
MOTS-c Research
MOTS-c & Thyroid Hormones / Uncoupling Proteins:
Bahar MR, et al. "Effects of intracerebroventricular MOTS-c infusion on thyroid hormones and uncoupling proteins." PubMed (2023)
MOTS-c: Metabolic Homeostasis & Insulin Resistance (Original Discovery Paper):
Lee C, et al. "The mitochondrial-derived peptide MOTS-c promotes metabolic homeostasis and reduces obesity and insulin resistance." Cell Metabolism (2015)
MOTS-c: Therapeutic Exploitation Review:
"MOTS-c: A promising mitochondrial-derived peptide for therapeutic exploitation." Frontiers in Endocrinology (2023)
MOTS-c & Autoimmune Diabetes / Immunoregulation:
Kong BS, et al. "Mitochondrial-encoded MOTS-c prevents pancreatic islet destruction in autoimmune diabetes." Cell Reports (2021)
MOTS-c: Stress, Metabolism & Aging Mechanisms:
"Mitochondria-derived peptide MOTS-c: effects and mechanisms related to stress, metabolism and aging." PMC (2023)
GHK-Cu Research
GHK-Cu: Gene Expression & Regenerative Actions:
Pickart L, Margolina A. "Regenerative and Protective Actions of the GHK-Cu Peptide in the Light of the New Gene Data." International Journal of Molecular Sciences (2018)
GHK-Cu: Skin Regeneration & 4,000+ Gene Modulation:
Pickart L, Margolina A. "GHK Peptide as a Natural Modulator of Multiple Cellular Pathways in Skin Regeneration." BioMed Research International (2015)
GHK-Cu: DNA Resetting & Genome Health:
Pickart L, et al. "GHK and DNA: Resetting the Human Genome to Health." BioMed Research International (2014)
GHK-Cu: Cognitive Health & Oxidative Stress Prevention:
Pickart L, Margolina A. "The Human Tripeptide GHK-Cu in Prevention of Oxidative Stress and Degenerative Conditions of Aging." Oxidative Medicine and Cellular Longevity (2012)
GHK-Cu: Nervous System Function & Cognitive Decline:
"The Effect of the Human Peptide GHK on Gene Expression Relevant to Nervous System Function and Cognitive Decline." PMC (2017)
Trace Elements & Thyroid Function
Copper & Thyroid Function:
"Trace elements and the thyroid." Frontiers in Endocrinology (2022)
Trace Elements in Thyroid Disease & Oxidative Stress:
"The Role of Selected Trace Elements in Oxidoreductive Homeostasis in Patients with Thyroid Diseases." International Journal of Molecular Sciences (2023)
Copper & Selenium in Thyroid Maintenance:
Kim MJ, et al. "Exploring the role of copper and selenium in the maintenance of normal thyroid function among healthy Koreans." Journal of Trace Elements in Medicine and Biology (2020)
Thyroid Hormone & Uncoupling Proteins
Thyroid Hormone & UCP Regulation:
"Thyroid hormone and uncoupling proteins." FEBS Letters (2003)
UCP1 & Central Thyroid Hormone Effects:
"Essential role of UCP1 modulating the central effects of thyroid hormones on energy balance." PMC (2016)
UCP Regulation & Turnover:
"The regulation and turnover of mitochondrial uncoupling proteins." PMC (2010)
Regulatory T-Cells & Autoimmune Disease
Tregs in Autoimmune Disease:
"Regulatory T cell function in autoimmune disease." PMC (2021)
Tregs: Therapeutic Potential:
"Regulatory T cells (Tregs) and their therapeutic potential against autoimmune disorders." Human Vaccines & Immunotherapeutics (2022)
Hashimoto's Disease Overview
Mayo Clinic - Hashimoto's Disease:
